 A fructose intolerance, also known as fructose malabsorption, is a type of digestive disorder that renders your body unable to properly digest the sugar from fruit.
A fructose intolerance, also known as fructose malabsorption, is a type of digestive disorder that renders your body unable to properly digest the sugar from fruit.
Normally, when you ingest fructose, the sugar gets broken down and absorbed. In cases of fructose intolerance, the fruit sugar gets eaten up and fermented by the bacteria living in your intestines.
Unfortunately, these bacteria tend to produce things like methane, short-chain fatty acids, and hydrogen when they ferment fructose.
These substances and gasses produce various unpleasant symptoms that can sometimes get confused with irritable bowel syndrome.
Understanding the symptoms of fructose intolerance in adults, which foods to avoid for fructose intolerance, and in general how to manage a fructose free diet will all be explained.
What Causes Fructose Intolerance?
Fructose intolerance has an assortment of different causes, though most of them are merely suspected rather than confirmed. Incidentally, although there are several similarities between irritable bowel syndrome and fructose intolerance, the rates of intolerance among IBS sufferers is not much different than those in the larger population, so it seems that IBS is at least not a significant risk factor. Other, more suspected causes include:
- An inherited abnormality with the fructose transport protein, GLUT-5. Fructose intolerances sometimes run in families.
- There is some association between fructose intolerance and toddler’s diarrhea, so it’s possible that an overuse of fruit juice (which causes the diarrhea) or high fructose corn syrup in early childhood could be involved.
- Damage to the intestinal lining, such as from chemotherapy or radiation, also shows associations.
- An overgrowth of bacteria in the small intestine may interfere with the ability to absorb nutrients, including fructose.
- Stress or inflammation may also possibly be a trigger.

Abdominal cramping is one main symptom of fructose intolerance. Other primary symptoms include bloating, gas and diarrhea.
How to Recognize if You Are Fructose Intolerant
The symptoms of fructose intolerance will vary in severity from person to person. The amount of fructose one individual needs to eat to trigger symptoms may be higher or lower than the next. The main symptoms are a result of the gases released during the fermentation process and most commonly consist of:
- Bloating
- Gas
- Abdominal cramping
- Diarrhea
Less common but still seen are:
- Fatigue
- Headaches
- “Brain fog”
- Mood swings
- Constipation
It’s difficult to self-diagnose a fructose intolerance since the symptoms overlap with those caused by irritable bowel syndrome, lactose intolerance, or other digestive disorders. A final diagnosis requires a proper test performed in a doctor’s office, and the fructose intolerance test is a process called the “hydrogen breath test.”
Basically, hydrogen and methane are two of the byproducts from your intestinal bacteria fermenting fruit sugars. Some of these gasses find their way back up the intestinal tract and into the stomach or throat. A hydrogen breath test can measure the levels of hydrogen and methane in your breath to see if the amount is consistent with those found in a fructose intolerance.
A hydrogen breath test is not as simple as, say, a breathalyzer, but it is a fairly simple and noninvasive procedure. The test begins with you drinking a solution of glucose and water and then breathing into a plastic bag. For adults, these breath samples are taken every 15 minutes. It can take up to three hours for the full set of breath samples to be taken and analyzed.
A hydrogen breath test can also be used to check for lactose intolerance, sucrose intolerance, and glucose intolerance, with the solution being the main component that changes depending on what is being tested for.
Hereditary Fructose Intolerance
The reason that fructose intolerance is also known as fructose malabsorption is to help avoid confusion with a condition known as hereditary fructose intolerance (HFI). Although both fructose intolerance and HFI are triggered by the same sugar, the effects are very different.
HFI is a genetic condition that is normally spotted during infancy. In cases of HFI, the body lacks an enzyme called aldolase B, which is needed to break down fructose. Without it, when the person eats fructose or sucrose, a series of chemical reactions takes place that not only damages the liver but also prevents the body from accessing its own glycogen stores. Blood sugar plummets and liver toxicity develops.
HFI has some distinctive symptoms that will start to appear when the infant begins eating solid foods or formula, including:
- Irritability
- Excessive sleepiness
- Poor feeding
- Vomiting
- Yellowed skin or eyes (jaundice, sign of liver issues)
- Enlarged liver or spleen
- Poor weight gain
- Convulsions
As with normal fructose intolerance, HFI cases can range from mild to severe. Effectiveness of treatments revolve around how soon the diagnosis is made, how quickly sucrose and fructose are removed from the diet, and how severe the aldolase B deficiency is.
How to Manage Fructose Intolerance
Fructose intolerance does not have a cure or medical treatment as of yet, so the only option currently available is to minimize the presence of fructose in the diet. Establishing a fructose intolerance diet plan is easier said than done, unfortunately. Fructose is naturally present in fruits, certain vegetables, and honey, in addition to table sugar and, of course, the high fructose corn syrup that is used in a spectacular assortment of processed foods and drinks.
Even many health foods can contain fructose. Due to this ubiquity, it’s important to figure out how much fructose your body can actually tolerate to get an idea of how strict your fructose intolerance diet is going to need to be.
A few quick tips to start off your management plan:
- Sorbitol can sometimes exacerbate the symptoms of fructose intolerance, but this isn’t always the case. Find out if you can eat foods with sorbitol.
- Consuming glucose alongside fructose helps improve your body’s ability to absorb (and thus tolerate) the latter. If you must eat food with fructose, aim for items with high glucose levels as well or take some glucose before the meal.
- Your body can handle small amounts of fructose better if taken after a meal rather than on an empty stomach.
Foods to Avoid if You Are Fructose Intolerant
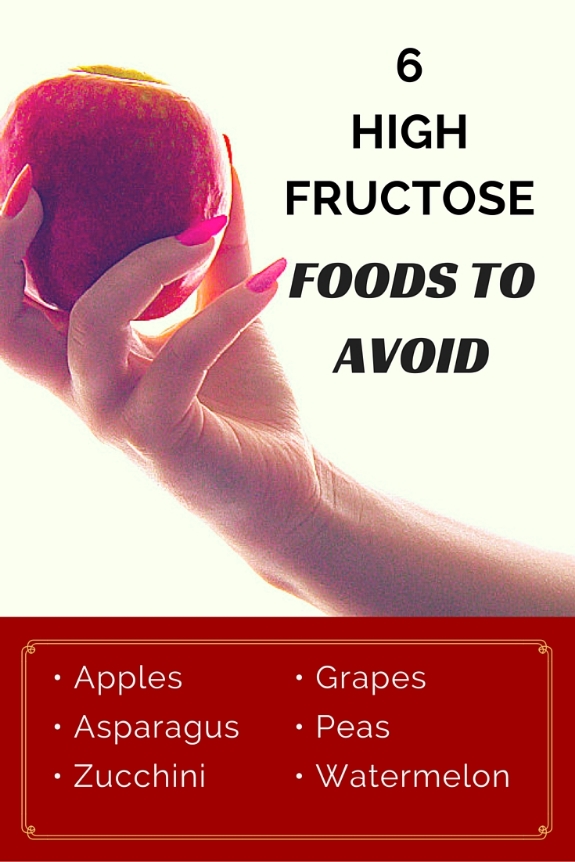
For obvious reasons, you will want to avoid foods that are high in fructose. These can include:
- Apples
- Asparagus
- Fruit juices
- Grapes
- Peas
- Watermelon
- Zucchini
Some foods contain fructose but in low enough amounts that you may be able to tolerate having them provided your intolerance isn’t severe:
- Avocados
- Bananas
- Blueberries
- Carrots
- Green beans
- Lettuce
- Strawberries
However, as mentioned above, fructose is found in numerous other products, dishes, and drinks, since it is a common additive. Even if not directly named (as in high fructose corn syrup), fructose finds its way into many different types of sweeteners and additives. When reading an ingredients list, stay away from any foods containing the following:
- Agave syrup
- Baker’s sugar
- Beet sugar
- Brown rice syrup
- Brown sugar
- Cane sugar
- Carob powder
- Corn syrup
- Date sugar
- Dulcitol
- Fruit juice sweeteners
- Grape syrup
- Gur
- Honey
- Maple syrup
- Molasses
- Polydextrose
- Stevia
- Turbinado
- Wasanbon
This is a long list, but it doesn’t cover every possible form of sweetener. The good news is that there are some sugars and sweeteners that your body can still tolerate. When trying to find foods you can eat with a fructose intolerance, look for anything that contains:
- Aspartame
- Barley malt syrup
- Birch sugar (pure)
- Corn starch
- Corn sugar
- Dextrin
- Erythitol (pure)
- Glucose
- Glucose polymers
- Neotame
- Saccharin
A Fructose Intolerance Diet Plan; Avoiding Fruit Sugar
When beginning your dietary adjustments, start by eliminating all or as much fructose as you can for two to four weeks. During this period, keep track of your symptoms (if any). Once this period passes, you can start introducing one new fructose-containing food into your diet every four days.
Slowly experiment to see which ones you can tolerate and in what amounts. In addition to the lower fructose fruits and vegetables listed above, here are some other candidates to consider for your introduction period:
- Cantaloupe
- Celery
- Chives
- Cucumbers
- Kale
- Kiwi
- Lettuce
- Oranges
- Pineapples
- Pumpkins
- Radishes
- Raspberries
- Rhubarb
- White potatoes
Continue to keep track of your symptoms and maintain a food diary as you start adding in fructose-containing foods. If you eat something that gives you a reaction, make a note of it and wait an extra few days before trying another reintroduction. Eventually, you will come up with a list of foods that you know your body can handle and will be able to create a more personalized diet plan based on your discovered tolerances.
When making your reintroductions, be mindful of foods that have high levels of fructose in them. Only attempt to eat one of these once you have been able to find some other less fructose-rich but more manageable foods to help build up your tolerance. Be mindful when attempting to eat the high fructose fruits and vegetables described earlier, along with:
- Applesauce
- Broccoli
- Cauliflower
- Cherries
- Corn
- Dried fruits (raisins, dates, etc.)
- Eggplant
- Garlic
- Mangoes
- Nectarines
- Pears
- Onions
- Pickles
Can You Prevent Fructose Intolerance?
Fructose intolerance has no known preventative methods or cure. Although adopting a diet plan like the one described above can help get your body more used to fructose and minimize symptoms, it’s possible for an intolerance to flare up again over time. Sticking to a low fructose diet plan can help reduce future severities, but there is not much information available about how effective this can be.
While fructose intolerance has no clear cause or prevention method, HFI does have a known cause and there are certain informative, but not necessarily preventative, measures that can be used. Genetic testing can reveal which parents, if any, carry a nonworking copy of the aldolase B gene. If both parents possess the gene, there is a roughly 25% chance of hereditary fructose intolerance being passed down to a child. While both parents being positive for the gene doesn’t automatically mean the child will have HFI, a negative test on either parent means that the kid is in the clear.

Fructose intolerance complications include liver failure, gout, and hypoglycemia.
Possible Complications of Fructose Intolerance
The good news, sort of, is that an unmanaged fructose intolerance is going to make your bowels spectacularly displeased but otherwise does not cause any serious complications.
However, the stress placed on your body from dealing with constant digestive difficulty can lead to various nonspecific issues ranging from electrolyte imbalances (from diarrhea) to mild rectal bleeding or an increased risk of anal fissures (from constipation). You would likely also experience recurrent trouble in focusing due to headaches, fatigue, cramping.
An uncontrolled hereditary fructose intolerance is a more serious matter. As mentioned earlier, HFI normally presents itself in infants and leaving the condition unrecognized or untreated can lead to host of possible complications. These include, but are not limited to:
- Liver failure, liver damage, or increased susceptibility to liver disease
- Gout
- Hypoglycemia (dangerously low blood sugar)
- Failure to thrive (difficulty or inability in gaining weight)
What This All Means
A fructose intolerance means you need to be extra careful about what foods you eat until you manage to determine just how much fruit sugar your body can tolerate. This will require a bit of experimentation but so long as you take a steady approach and don’t add too many new fructose foods at once, you should be able to determine a good dietary balance that works.
For parents of small children, the idea of a hereditary fructose intolerance can seem scary, but it’s quite possible to catch it before any serious complications develop. Simply paying attention to your child, especially to any odd behaviors or symptoms that appear alongside feeding, can help you detect potential symptoms and prompt you to seek a formal diagnosis.
Sources for Today’s Article:
“Hereditary Fructose Intolerance,” Medline Plus web site, last updated April 5, 2016; https://www.nlm.nih.gov/medlineplus/ency/article/000359.htm, last accessed April 20, 2016.
Zeratsky, K., “Fructose intolerance: Which Foods to Avoid?” Mayo Clinic web site, March 6, 2014; http://www.mayoclinic.org/fructose-intolerance/expert-answers/faq-20058097, last accessed April 20, 2016.
“Hydrogen Breath Test,” University of Michigan Health System web site, September, 2015; https://www.med.umich.edu/1libr/aha/umhbt.htm, last accessed April 20, 2016.
“Fructose Intolerance,” Diet web site; http://www.diet.com/g/fructose-intolerance, last accessed April 20, 2016.
