 What is known to some as a double whammy, psoriatic arthritis carries similar traits to rheumatoid arthritis.
What is known to some as a double whammy, psoriatic arthritis carries similar traits to rheumatoid arthritis.
It affects the joints, sometimes on one side of the body or both, and it presents with skin lesions in many patients.
In fact, a whopping 30% of psoriasis cases result in psoriatic arthritis, according to the Arthritis Foundation.
There are many cases in which inflammation of the joints begins before any signs of the red, scaly rash. Psoriatic arthritis symptoms do not discriminate and can be seen with any gender and age, though it is less common in young people. This condition is linked with spondyloarthropathies, chronic joint diseases that cause spine inflammation. Inflammation can develop in the tendons, cartilage, eyes, the lining of the lungs, and the aorta, although rare. We will examine the causes and if psoriatic arthritis treatment exists.
Types of Psoriatic Arthritis
Psoriatic arthritis is an autoimmune disease that affects the joints and skin when healthy tissue is attacked by our immune system. There are five types of this condition.
1. Symmetric Psoriatic Arthritis
This form of psoriatic arthritis directly affects joints on both sides of the body, similar to rheumatoid arthritis. It is estimated 50% of patients are diagnosed with this type.
2. Asymmetric Psoriatic Arthritis
This version is not present in the same joints on opposite sides of the body at the same time. This affects 35% of psoriatic arthritis patients.
3. Distal Psoriatic Arthritis
This type directly targets the ends of your fingers and toes with inflammation and stiffness. Your nails can also have white spots, pitting, and separate from the nail bed.
4. Spondylitis
This form of psoriatic arthritis refers to pain and stiffness in the neck and spine regions.
5. Arthritis Mutilans
The condition affects five percent of patients with the classification of being the most severe form as it causes abnormalities with the toes and fingers smallest joints. It can result in destroying the end joints of the digits.
What Causes Psoriatic Arthritis?
Unfortunately, there is no concrete cause for this condition. It can be caused by the immune system failing, environmental factors, genetic traits, or a combination of these.
Some studies show a family gene may be responsible for the reason 40% of patients have family members who are also diagnosed with psoriatic arthritis. There is research linking a trigger such as an infection as a possible connection for those relations at risk. This has lead researchers to suggest there may be various infections involved such as psoriasis bacteria.
For others, the psoriatic arthritis presents itself after an infliction from an injury or accident directly to a joint. It is thought the stressed and overworked immune system begins attacking the joint tissues. Again, this seems to happen in those with a genetic risk.
Psoriatic arthritis is not transferable, but some research does show a link to strep throat. The immune system of those with reduced helper T cells, such as in HIV and AIDS patients, seems to be involved with symptoms of psoriatic arthritis as well.
Psoriatic Arthritis Symptoms
As a chronic disease, psoriatic arthritis can also present symptoms that appear to improve and sometimes disappear for periods at a time before returning. The symptoms may be mild or more severe each time they reappear.
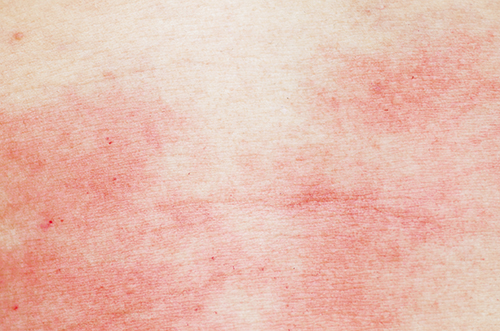 1. Skin Rash
1. Skin Rash
As it is directly linked to the skin condition psoriasis, in most cases, you may develop flaky, thick, red skin surrounding silver-white scaly skin patches.
2. Swollen Digits
Your fingers and toes can swell to resemble sausages with severe pain as the joints and tendons become inflamed. Some patients will present with hand and foot deformities long before the joints are directly affected.
3. Nail Changes
You may see changes in your toenails and fingernails such as discoloration, thickening, and pitting.
4. Foot Pain
Pain can appear on the heel and sole of feet where the tendons and ligaments meet the bone.
5. Stiffness
The range of motion is reduced and ability to move your joints easily may be tampered with stiffness and accompanying pain.
6. Back Pain
Pain in the lower back is a sign of spondylitis, caused by psoriatic arthritis. The joints of your vertebrae and in between the spine and pelvis become inflamed.
Fatigue
Psoriatic arthritis can cause fatigue from the physical and emotional exhaustion of dealing with the disease.
Focusing on mainly the joints and skin tissue, psoriatic arthritis does not directly target any vital organs. However, it can cause inflammation of the eye. This painful condition, known as uveitis, affects the front of your eye and calls for immediate medical attention.
How is Psoriatic Arthritis Diagnosed?
Expect your doctor to put you through a series of tests to rule out other types of arthritis such as rheumatoid arthritis and the condition of gout. This will include examining your nails for discoloration and pitting and your joints for any tenderness and swelling. The soles of your feet will also be checked for tenderness.
Other tests may look for joint, tendons, and ligaments issues by using X-rays and magnetic resonance imaging, known as a, MRI test. This projects images of the body tissues.
Lab tests are used to detect psoriatic arthritis. Checking for the rheumatoid factor in the blood will distinguish between the similar symptoms of the two conditions of psoriatic arthritis and rheumatoid arthritis. By removing joint fluid with a needle, your doctor will test for any signs of uric acid crystals, which reflect the condition of gout rather than psoriatic arthritis.
What Are the Risk Factors?
Research on determining who is at the greatest risk of developing psoriatic arthritis has conflicting results with one common dominator, psoriasis.
The Mayo Clinic website states that having psoriasis is the “single greatest risk factor for developing psoriatic arthritis. People who have psoriasis lesions on their nails are especially likely to develop psoriatic arthritis.”
Chief editor of Medicine Net, William C. Shiel Jr., MD, FACP, FACR, writes, “The major risk factor for developing psoriatic arthritis is having a family member with psoriasis.”
Both sources refer to the skin condition psoriasis as being directly involved in the likelihood of developing psoriatic arthritis.
Medications and Home Remedies for Psoriatic Arthritis
A variety of prescribed and over-the-counter drugs can be used as treatment for psoriatic arthritis.
- Immunosuppressants help to control the immune system, which functions abnormally during psoriatic arthritis. Azathioprine and cyclosporine drugs can put you at higher risk for infection.
- Disease modifying antirheumatic drugs, or DMARDs, aid in reducing the progression of the condition by prevent further damage to the tissues and joints. These include methotrexate, leflunomide, and sulfasalazine. They may have the side effects of lung infections, liver damage, and bone marrow suppression.
- TNF alpha inhibitors stimulate our body’s production of the inflammatory matter of TNF alpha. Etanercept, infliximab, adalimumab, golimumab, and certolizumab all reduce pain, swelling, and stiffness. Side effects can include hair loss, nausea, diarrhea, and increase your risk for infections.
- Nonsteroidal anti-inflammatory drugs, known as NSAIDs, suppress inflammation and mild pain. You can purchase ibuprofen such as Advil and Motrin and naproxen sodium pills such as Aleve at your local pharmacy. Your doctor may need to prescribe NSAIDs for more severe pain. NSAIDs have side effects of heart issues, liver and kidney damage, and stomach irritation.
There have been introductions of medication to the market recently such as apremilast, ustekinumab, and secukinumab.
Other options your doctor may offer include steroid injections to reduce inflammation and joint replacement surgery. This surgery replaces damaged joints with metal or plastic artificial prostheses.
Home Remedies
To prevent further damage to your joints and maintain good joint health, these daily activities and lifestyle behaviors can be followed at home.
 1. Regular Exercise
1. Regular Exercise
It is just as important for your joints and muscles to be regularly worked as it is your entire body. Avoid exercises that put strain on your joints. Swimming, walking, and biking are joint-friendly.
2. Weight Maintenance
To alleviate any strain on joints, maintain a healthy weight. By eating a nutrient enriched diet of plant-based foods, you will also help to keep your body components strong and healthy.
3. Rest
The inflammation and pain of joints can result in exhaustion, as does some medications. Take short breaks while working or performing daily activities.
4. Joint Protection
To prevent joint damage, or to lessen the damaged done, protect your joints throughout the day by changing the way you complete tasks. Use jar openers instead of your hands, always use both hands to lift heavy objects such as cooking pots, and use your body to push open doors rather than your fingers.
5. Support
The emotional toll psoriatic arthritis can cause on a person is sometimes overwhelming. Pain and lack of mobility can create an internal environment that has the patient feeling down and lonely. It is important to have the support of family and friends as much as the professional medical support. Join a support group and talk to a therapist to manage stress to avoid stimulating the psoriatic arthritis.
Psoriatic arthritis, like many conditions, can inflict physical, mental, and emotional pain on a person. The pain and swelling of joints, along with skin lesions, can create an environment of isolation. With no direct cause or cure for this debilitating disorder, it is vital to seek medical advice with any signs of symptoms. Medications, exercises, physical and emotional therapy, and the support of family and friends offers assistance for maintaining a healthy, normal life.
Related:
- Essential Oil for Arthritis: 10 Essential Oils That Help Relieve Arthritis Pain
- 5 Herbs for Arthritis in the Hands and Knees
- Three Hand Exercises for Joint Pain Relief
Sources:
Shiel Jr, William, MD, FACP, FACR, “Psoriatic Arthritis,” Medicine Net; http://www.medicinenet.com/psoriatic_arthritis/article.htm#psoriatic_arthritis_facts, last accessed February 6, 2017.
“Psoriatic Arthritis,” Arthritis Foundation; http://www.arthritis.org/about-arthritis/types/psoriatic-arthritis/, last accessed February 6, 2017.
“Psoriatic Arthritis,” Mayo Clinic; http://www.mayoclinic.org/diseases-conditions/psoriatic-arthritis/home/ovc-20233896, last accessed February 6, 2017.
